My Lab: Specialist testing services
Leeds Teaching Hospitals Trust (LTHT) is one of the largest NHS trusts in the country.
It includes Leeds General Infirmary, the second largest major trauma centre in the UK, and St James’ University Hospital, home to the Leeds Cancer Centre and one of the UK’s largest solid organ transplantation centres. We also supports the Leeds Children’s Hospital, which provides specialist care for children up to the age of 16. In addition, we provide antenatal screening services to clinics and communities of the West Yorkshire region. As part of the regional pathology modernisation initiative, LTHT is one of six trusts within the West Yorkshire Association of Acute Trusts (WYAAT), with the main pathology hub based at LTHT.
Our new pathology laboratory is currently under construction at our St James’s site and will complete next year. With new, state-of-the-art technology and equipment, it will support the delivery of pathology services right across West Yorkshire and Harrogate.
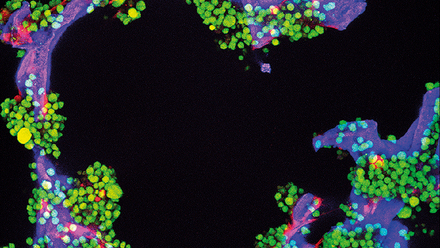
Leeds is one of few remaining “stand-alone” blood transfusion laboratories outside of NHS Blood and Transplant (NHSBT). Therefore, we undertake specialist testing services not offered by many other service providers. LTHT Blood Bank offers exposure and training in niche blood transfusion techniques and complex patient serology. We primarily use Grifols technologies, but also impart our own serological expertise using an array of carefully selected antibody panels, elutions, and antibody neutralisation techniques.
Over the past year, our laboratory has processed 75,000 ABO/RhD group and antibody screens, issued 26,000 red blood cell units and 5000 plasma components with an additional 7800 platelet units. These were utilised as part of routine patient testing and 1748 life-saving major trauma events, including 53 of those within our own delivery suite theatres. We also participate in UK NEQAS serology and fetomaternal haemorrhage (FMH) exercises, and NHSBT IPEx.
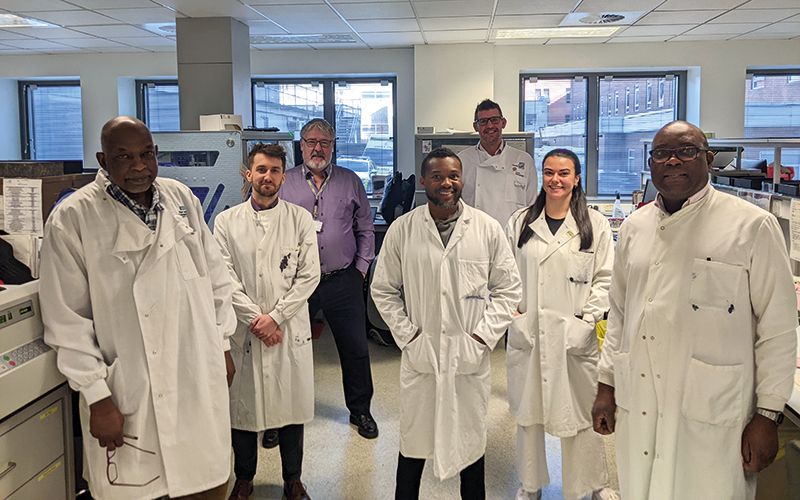
What sets LTHT apart from other laboratories is our close collaboration with other allied healthcare professions and services. Recently, laboratory staff were invited to take part in major haemorrhage simulations within A&E, paediatric and delivery suite theatres. Here, staff actively engaged and stress-tested existing patient safety pathways for the purpose of quality improvement. Our aims for the next year include inviting patients from haematology/oncology treatment centres to visit the laboratories to experience the analytical testing process, and to share their past experiences.
Before COVID-19, we had arranged similar experiences through Harvey’s Gang, an initiative that shared the same vision with chronically ill children, providing them with opportunities to take part in their own journey throughout our clinical laboratories. This was a staff favourite and one of many means of promoting patient-centric care within a laboratory setting. Other recent successes include the rollout of Blood Track Tx, which has seen 2000 clinical staff trained within a six-month period and an 80% reduction in patient re-bleeds. We are also moving to a new laboratory information management system (LIMS) and decanting to a temporary laboratory, while our existing one is improved ready for the future of WYAAT services in our “hub and spoke” consolidation of services.
Leeds has the potential to offer a lot of career development opportunities. We have individuals enrolled on vocational courses provided by the IBMS and British Blood Transfusion Society (BBTS), with others studying at Masters level. We have our first intake of the Scientist Training Programme (STP) and Higher Specialist Scientist Training (HSST) candidates in haematology and blood transfusion; thus, opening new avenues in facilitating and engaging patient care pathways. Current pre-registrant biomedical scientists are expected to engage service users through their portfolios – whether related to service improvement, or applying new skills to promote patient-centred care.