Laboratory transfusion standards
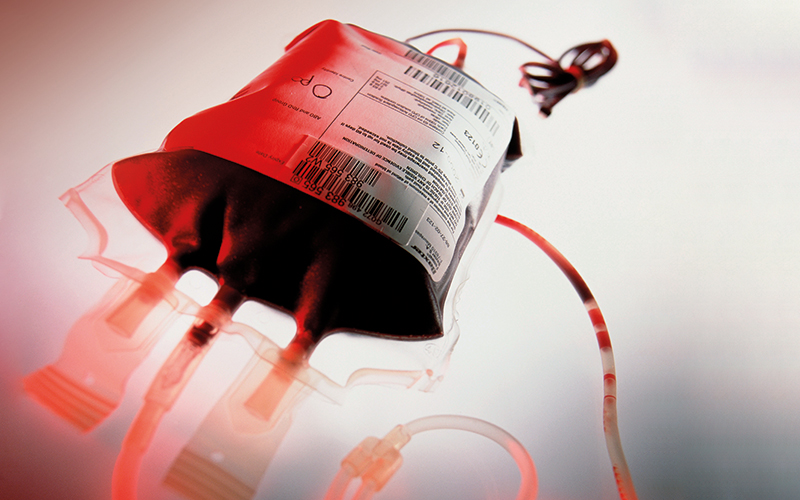
Blood transfusion laboratory practice is heavily regulated due to the potential to cause serious harm or death to patients. When adverse events occur, there are far-reaching consequences affecting the patient, the family and causing an emotional and professional impact on staff involved and impacting the organisation’s reputation. Transfusion in the UK remains relatively safe, with a transfusion-related risk of death of 1 in 53,193 and of serious harm of 1 in 15,142 components issued in the UK, according to the 2020 Serious Hazards of Transfusion (SHOT) report. However, avoidable errors account for the majority of errors. The 2021 SHOT report states laboratory errors and near-miss events accounted for 18.1% of all SHOT reports in 2021.
The UKTLC’s background
In 2006 it was recognised that there were recurrent deficiencies in transfusion laboratories across the UK resulting in unacceptably high levels of reports submitted to SHOT. The SHOT team launched an initiative working with the British Blood Transfusion Society (BBTS), IBMS, Royal College of Pathologists (RCPath), UK National External Quality Assurance Scheme (UKNEQAS) and the NHS England National Blood Transfusion Committee (NBTC) and its equivalents in Scotland, Wales and Northern Ireland, which led to the formation of the UKTLC.
The UKTLC principally aims to:
- promote dialogue between the collaborative stakeholder organisations to achieve and maintain a consistent advisory approach for organisations invested in achieving and/or maintaining the regulations and standards for transfusion practice as outlined by but not limited to the Blood Safety and Quality Regulations (BSQR), the Good Practice Guidelines (GPG), Joint UK Blood Transfusion and Tissue Transplantation Services Professional Advisory Committee (JPAC) and the British Society for Haematology (BSH)
- influence positive changes within the transfusion community through the collaborative identification and promotion of best practice
- provide a collaborative forum able to deliver guidance to the UK transfusion community to improve patient safety and care within transfusion
- publish national standards in relation to staff education, qualifications, knowledge and competency within UK transfusion laboratories
- provide a framework for transfusion laboratory staff capacity planning and staff mix.
Development of standards
To understand the status of laboratory practices and the challenges faced by those working in transfusion the UKTLC carried out surveys in 2007 and 2008 that revealed a lack of formal transfusion knowledge, that lead transfusion scientists were not available in core hours due to shift working and that most laboratories with agreed capacity plans were routinely running services below the levels required by their own plans.
In the absence of any formal guidance in 2009 the UKTLC developed a series of recommendations that were designed to help hospitals achieve the minimum standards of proficiency and practice set by the Health and Care Professions Council (HCPC) and the Blood Safety & Quality Regulations (BSQR 2005). These standards defined the minimum expectations for staff levels, skill mix, qualifications, training and competency, and the use of information technology. This level of clarity in the requirements for safe practice had not been available previously and provided management with a tool to benchmark against a gold standard.
Challenges continued with the recruitment of suitably trained scientists.
It was hoped that compliance with these recommendations would lead to a significant reduction in transfusion laboratory errors, however, a 2012 SHOT report indicated an error reduction rate of only 12%, far below the 50% agreed and expected following the 2009 recommendations for best practice.
A 2013 UKTLC survey demonstrated that a significant number of laboratories had not addressed many of the recommendations and that IT errors appeared to be increasing. The general view was that “although the recommendations were excellent, management saw them as recommendations that carried no mandatory action requirement”. To counter this in 2014, the recommendations were redrafted as evidence-based standards supported by the Medicines and Healthcare products Regulatory Agency (MHRA) to be used by the inspectorate as part of the inspection programme. Later, the UK Accreditation Service (UKAS) also came to adopt the standards for accreditation purposes in transfusion laboratories.
The 2023 standards
A 2019 UKTLC report noted that challenges continued with the recruitment of suitably trained biomedical scientists, and with funding and time for training and education.
A survey of laboratory culture in the same year noted that some staff felt under pressure to present an unrealistic impression of their laboratory’s compliance with the GPG to appear more in line with the BSQR and the MHRA’s blood compliance report. The report exposed the pressures affecting staff and raised the importance of a just culture in the provision of a safe service. The COVID-19 pandemic saw further challenges for transfusion laboratories and the wider health service, particularly in terms of staffing, recruitment and training.
All this has led to the UKLTC spending the last year revising and updating their standards. The UKTLC now includes representatives from the IBMS, MHRA, NHSBT, the NHS in each of the four home nations, RCPath, SHOT, UKNEQAS and UKAS, all of whom have contributed to the review of the minimum standards.
The 2023 revision updates the recommendations, considering current and future changes in blood transfusion laboratory practice. They provide a minimum level of standards, focusing on patient safety and key areas of practice and core skills for staff. The UKTLC aimed to provide a set of updated standards that were pragmatic and realistic for implementation whilst continuing to improve patient safety and support laboratory staff.
The standards fall into four areas
- Staffing: Including staffing levels, capacity planning, quality management systems and appropriate specialist staff
- Qualifications, knowledge and skills: For Scientists at Band 7 and above, Scientists at Band 6 and Band 5, Scientists in training and support staff, Staff supporting the Blood Transfusion Service, training and competency assessment and resources for training
- Information technology: Analysers, Laboratory Information Management Systems (LIMS) and Electronic Transfusion Systems
- A just culture: Staff should be encouraged to report errors, near-miss events, suggestions for improvements and potential risks that may affect patient safety. Processes for reporting, and learning from, excellence and incident investigation processes, which must include consideration of human factors and systems thinking, avoiding application of blame on individuals.
It is crucial staff are provided with the knowledge and skills to perform their roles effectively
Minimise risk
The standards are targeted at blood transfusion consultant leads, pathology directors, blood transfusion laboratory managers, operational managers and blood transfusion focused groups and should be used to support safe practice. The standards can be used to benchmark and then escalate staffing and IT issues supported by an evidence-based approach. They should be used in conjunction with guidance relating to transfusion laboratories at individual organisation level or within pathology networks.

It is expected that they will help minimise the risk of laboratory errors, through supporting and encouraging effective and appropriate education, training, competency assessment and utilisation of staff, and the use of technology in hospital transfusion laboratories within the current UK legislative requirements for blood transfusion services. These revised standards are supported by the IBMS and the RCPath and will be utilised in regulatory inspections by the MHRA and assessments under ISO 15189 standards by UKAS.
To help transfusion laboratory staff and management use the new standards in 2023 the UKTLC plans to increase its social media presence, taking part in online education events and developing practical support and resources for lab managers. A gap analysis tool, capacity plan examples, guidance for matching equivalency to IBMS qualification learning outcomes will be published on the UKTLC webpage hosted by SHOT, along with the results of the 2022 UKTLC survey.
The UKTLC purpose and vision is to support laboratory staff and improve safe transfusion practice. This is carried out by providing tools such as the UKTLC standards and survey findings. The UKTLC is modernising its approach and would be keen to hear ideas from laboratory managers regarding ways that the UKTLC could help improve safety and support laboratory staff within their remit. You can find the UKTLC on Twitter or contact one of this article’s authors.
In the ever-changing healthcare environment, with a backlog in workload and advancing technology, it is crucial that laboratory staff are provided with the knowledge and skills to perform their roles
effectively. Safe practice must be supported with access to adequate equipment and IT. The UKTLC standards provide the backbone on which a safe transfusion service must operate.
Kerry Dowling is Transfusion Laboratory Manager at University Hospital Southampton NHS Foundation Trust and Chair of UKTLC. Jennifer Davies is Transfusion Laboratory Manager, Royal Devon University Healthcare NHS Foundation Trust and Deputy Chair of UKTLC