Meet Amy

How Amy started out
"I completed my BSc in Medical Biochemistry and an MSc in Health & Clinical Sciences at the University of Surrey, before starting as a Medical Laboratory Assistant in Blood Sciences at Frimley Park Hospital in May 2015.
Since my Biomedical Science degree wasn’t IBMS Accredited, I had to have it assessed by the IBMS. Luckily, I did about 95% of the same modules as the accredited biomedical science degree, so didn’t have to do any top-up modules.
I started my IBMS Registration Portfolio in July 2016 as a Medical Laboratory Assistant and was appointed as a Trainee Biomedical Scientist in Haematology and Transfusion in September 2016.
I passed my verification in July 2017, and became a Specialist Biomedical Scientist in December 2019. In June 2020, I became a Senior Biomedical Scientist in Haematology."
What is haematology?
Biomedical scientists investigate the formation, composition, function and diseases of blood.
Some diseases diagnosed in haematology are leukaemia, malaria and anaemia. They also identify blood groups for blood donation, ensures the correct grouped blood is matched to the patient due to receive the donation and makes sure blood stocks are adequate for critical incidents such as road traffic accidents, operations and cancer treatments.
What does a typical day in your department look like?
"As a Senior Biomedical Scientist, I’m responsible for the efficient running of the laboratory and ensuring that we’re meeting ISO15189 standards with regards to quality and processes.
Day-to-day I could be reviewing “SOPs” or standard operating procedures. These are guidelines which we follow when working with a specific analyser or manual test.
SOPs provide useful information regarding:
- Troubleshooting methods
- Training new members of staff
- Inputting and checking External Quality Assessment results. (These get compared against other laboratories’ results across the country.)
- Verifying new lot numbers of reagent.
As I’m so new to the role there’s still a lot to learn and every week I’m doing something new."
The Night Shift
"This is the first of three nights for me, then I’ll get two days off. During the week there are two biomedical scientists on the night shift, one in Haematology and one in Blood Transfusion."
21:45
"I arrive at work for my night shift and get the hand-over from the late shift. There’s a few urgent blood films to look at and one of our analysers is giving dodgy results, so they’ll be first on my list tonight."
02:00
"Time for a cup of tea and a snack.
Most of the last 4 hours has been spent validating and authorising full blood counts and coagulation results.
Technical validation involves asking ourselves questions like “is this result feasibly possible from our analysers?” Whereas authorisation takes into consideration clinical details and patient history - so this involves asking questions like “Does this fit with what I know or has this changed significantly?”
Anything grossly abnormal will get a blood film to check that the results are genuine and not caused by artifactual occurrences like platelet clumps or myeloperoxidase (MPO) deficiency.
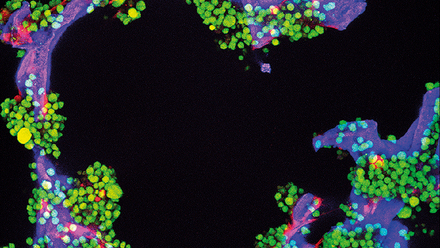
We use blood films to see a snapshot inside the patient. A small quantity of blood is smeared on a glass slide and stained so that we can see the red and white blood cells and platelets.
It allows us to look at the shape and size of the red cells (which can help us spot anaemia), the presence of immature white cells (which can indicate infection), or the presence of blast cells (indicating leukaemia).
Artifactual results, like platelet clumps, will only ever be seen by the analyser, and don’t reflect what happens inside the patient. Some patient’s platelets stick together when exposed to EDTA, the anticoagulant used for full blood counts, and this causes their platelet count to be low. By looking at a film, we can spot these clumps.
Whilst we can’t report a number, we can at least give an indication to the requesting clinician whether we think there are sufficient platelets present and advise them to send a paired EDTA and sodium citrate sample for the next FBC. Sodium citrate does cause the same clumping phenomenon and so we use this sample for platelet quantification!
MPO, or myeloperoxidase, is an enzyme found inside the granules of myeloid lineage white cells e.g. neutrophils. The analysers at my laboratory, Siemens ADVIA 2120s, used a methodology where the MPO staining and size of a cell is used to categorise it.
If a patient is MPO deficient, they have a genetic mutation where their granules lack the enzyme and the analyser can’t quantify the neutrophils properly. If this is the case, we use the blood film to do a manual white cell differential and visually count and categorise the white cells present."
06:00
"I get to sit down for the first time in a few hours to do more validating.
I’ve maintained 3 analysers so far and tried to troubleshoot the dodgy one from earlier. I have tried washing it, priming the reagents in case there’s air trapped in the lines, leaving it to soak in cleaning solution for extended periods of time in case the reaction chambers are dirty, and have finally logged the issue with an engineer.
The out of hours engineer has talked me through all the things I’ve done to try and rectify the situation and thinks we may need a new part which we don’t hold as stock in the laboratory. As the analyser has not passed its daily Quality Control (QC) checks, it’s kept out of use, and I’ll hand it over to the day staff.
I also have to make an urgent film on a patient with pancytopenia, which will be referred to the Haematology Consultants after I’ve checked the results are genuine."
08:15
"Home time!
Hand over to the day shift, including handing over the troublesome analyser. There’s very little outstanding work, so at least they’ll have the morning to sort it out before the GP work starts coming in and the work starts again."
What do you most enjoy about the role?
"Whilst the job can be demanding (especially overnight) I find it incredibly rewarding and love what I do. Every day brings something different, and there’s always an opportunity to learn new things.
I left university wanting to be useful and I’m definitely doing that!"
Looking to the future
"Even in the 5 years I’ve been in the lab I’ve seen the move to digital morphology change how we refer blood films, I think the consultants appreciate being able to see blood films on urgent results that we call at 3am before having to come in!
With the consolidation of labs into networks, I think we may see the loss of some specialisation at the hub labs, but that just means that rotation throughout the network becomes more important, so we don’t lose skills."