Under the microscope: microbiology and infection

AMR remains on the national risk register, which indicates drug-resistant infections are predicted to lead to 10 million deaths worldwide annually by 2050. The potential consequences within medicine are perhaps the most obvious where increased prevalence could impact areas such as routine surgery, and treatments such as chemotherapy may become more complicated. Clinical decision-making and patient care pathways will likely be affected and we could enter a scenario where some routine interventions will need to be re-evaluated as risks begin to outweigh potential benefits.
Resistance will inevitably increase if left unchecked. Nearly 100 years of well-documented antimicrobial usage has made that clear to anyone who has even a passing familiarity with the subject.
The morning sessions of this year’s conference will focus on discussing the complexity of the issue of AMR, beginning with our Keynote speaker Professor Alasdair MacGowan. Professor MacGowan, who is a consultant at the North Bristol NHS Trust, will give an overview of the development of AMR and discuss approaches for control.
Given his longstanding research interest in various aspects of antimicrobial stewardship and antimicrobial pharmokinetics, and as a former President of the British Society of Antimicrobial Chemotherapy, he has a long association with this subject.
Wider perspective
Dr Mandy Wootton from Public Health Wales will then provide an update on laboratory diagnostics in relation to the detection of AMR. Taking a wider perspective, Dr Claire Gordon will take a look at AMR surveillance in low- and middle-income countries. The burden of infection and impact of AMR still currently falls greatest on areas where resources are more limited. Diagnostics, surveillance and treatment are all harder to implement and maintain when they are competing for already limited available resources. However, as SARS-CoV-2 showed elegantly and brutally, pathogens are not bound by human borders. Transmission in today’s interconnected, globalised environment can happen with astonishing rapidity and certainly quickly enough to challenge the speed of political response.
As SARS-CoV-2 showed elegantly and brutally, pathogens are not bound by borders
Emerging technologies
Dr Nathaniel Storey, a bioinformatician who has significant experience in next-generation and other rapid sequencing techniques, will be able to discuss the advantages and present-day limitations of these approaches and give us some insights into the timescale for their adoption by the diagnostic laboratory.
Reflecting the eclectic nature of developments in microbiology, the afternoon session will deliberately move away from AMR and will contain a number of standalone talks from specialists in their fields.
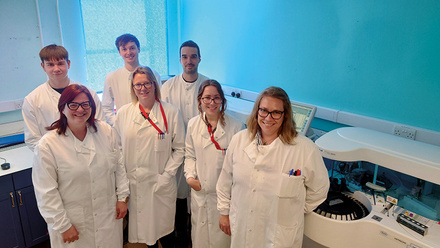
Michael Perry will provide a perspective on the network-wide implementation of molecular enteric techniques in Wales. The network approach to pathology is becoming more widespread throughout the UK, and Wales has embraced this on a national scale through continuation and development of the national pathology network following the break-up of the Public Health Laboratory Service in 2003. This provides the framework for standardising methodology (contributing to the UK-wide Standards for Microbiology Investigations programme) as well as equipment procurement pathways with collaboration and coordination between traditional geographic and professional areas of responsibility.
Orthopaedic infections
An area where there are significant limitations with traditional culture-based techniques is in the detection of orthopaedic infections. Low pathogen numbers and their stubborn adherence to surfaces, either native or prosthetic, results in low sensitivity and significant skill and time are required to do these important investigations well. Enrichment cultures seek to increase the sensitivity to detect pathogens, but require extended incubation and these can be prone to contamination, producing misleading and difficult-to-interpret results. One potential solution is the use of molecular methods and Dr Kevin Cole, a Senior Biomedical Scientist from North Tyneside General Hospital in Newcastle, will discuss both the advantages and disadvantages to this approach.
Necessary developments
Next-generation sequencing is an enticing prospect and potentially a powerful new tool in the diagnosis, management and treatment of infections, with further implications from an infection control or outbreak management perspective. Although new technologies may represent an intimidating looming threat to those more comfortable with traditional bacteriology, it is necessary that the advantages are widely discussed, and the current and future workforce is engaged in these developments. The arguments in favour may be clear in terms of the outcomes achieved, but getting to a position where these are fundamentally ingrained in routine diagnostic microbiology departments will no doubt present significant challenges.
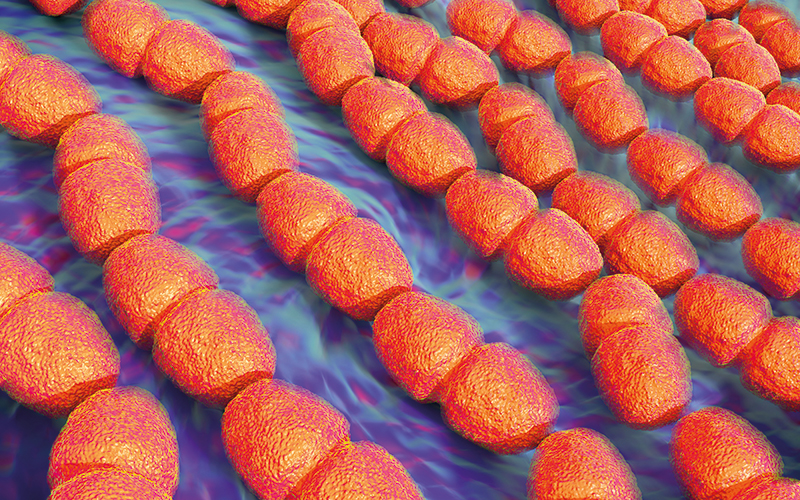
Group A Streptococcus
As COVID waned, other respiratory infections seem to rear up with renewed enthusiasm. This may be due to the effects of reduced social mixing during periods of lockdown, immune reductions or more pathogenic strains emerging. One pathogen that has made regular appearances in the mainstream media in recent months is Group A Streptococcus (GAS), leading to a flurry of diagnostic activity. Did this represent a true increase in the prevalence or severity of infection, or was it more driven by the increased media exposure to a few tragic cases? Dr Charlene Rodrigues, our last speaker, will conclude the meeting with an update on this current outbreak and discuss the behaviour of GAS and other respiratory infection in children in this “post-pandemic” period.
Attend the conference
For more information about the conference, which will take place in Hendon on 11 May, visit bsmt.org.uk.